Millennial-Inspired Nursing References Are Here to Stay
Nurses must prepare for a world in the near future where mobile devices are the sole communication tool for the healthcare team and patient or family. Mobile-only users have been on the rise over the last few years. In fact, mobile technologies are already widely adopted for personal health. Mobile apps make managing health customizable and convenient for patients with chronic health conditions and help people achieve personal health goals.
How do apps help nurses?
There is an urgent need for better nursing resources in fast-paced and changing clinical environments, and bring-your-own-device (BYOD) approaches to manage workspaces are becoming commonplace. The CDC says that health care information should be “accurate, accessible, and actionable”. Providers are trying to navigate the vast amount of health teaching targeting patients who frequently consult “Dr. Google” for advice, so that patients have accurate info. Then, why are nurses still using Google to find info?
The use of smart phones and tablets near or at point of care (POC) to support just-in-time (on-demand) learning is a hot debate. Of course, accessing online references at the nurses’ station is a necessity, and most resources are tucked into the electronic medical record and organized for physician consumption. Reviewing competencies, fact check policies, or guide nursing procedures, though, is not typically on the menu. But what about the learning organization and continual transformation to meet actual needs?
Nurses are continual learners and are known for seeking information to improve care delivery throughout their shift–it's part of nursing safety culture. Yet, we have trouble finding resources for what WE do. Access to valuable nursing information just makes sense for improving patient outcome, and the time has come for practical nursing references!
Nursing Reference Apps offer efficiency giving nurses more time with patients.
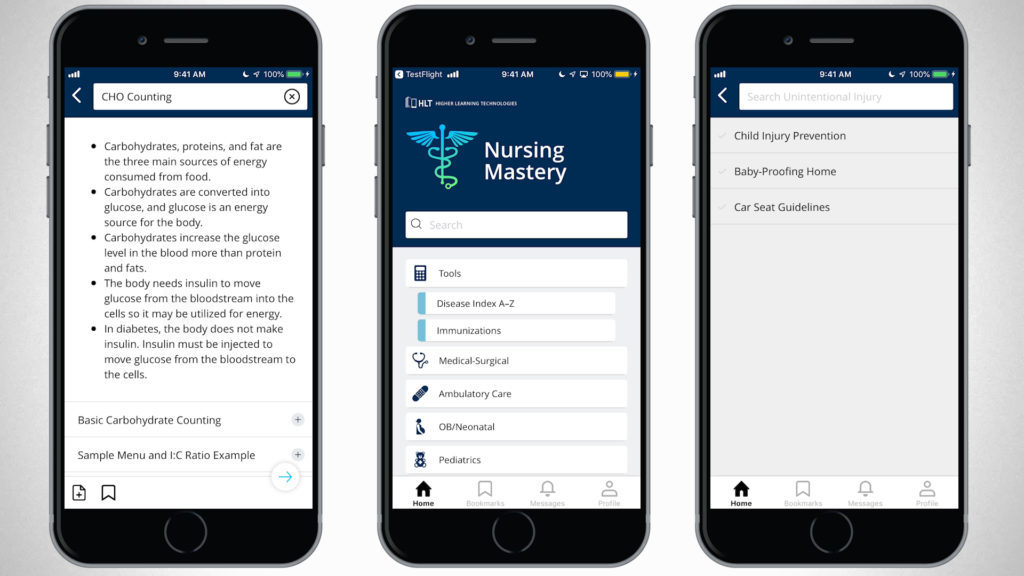
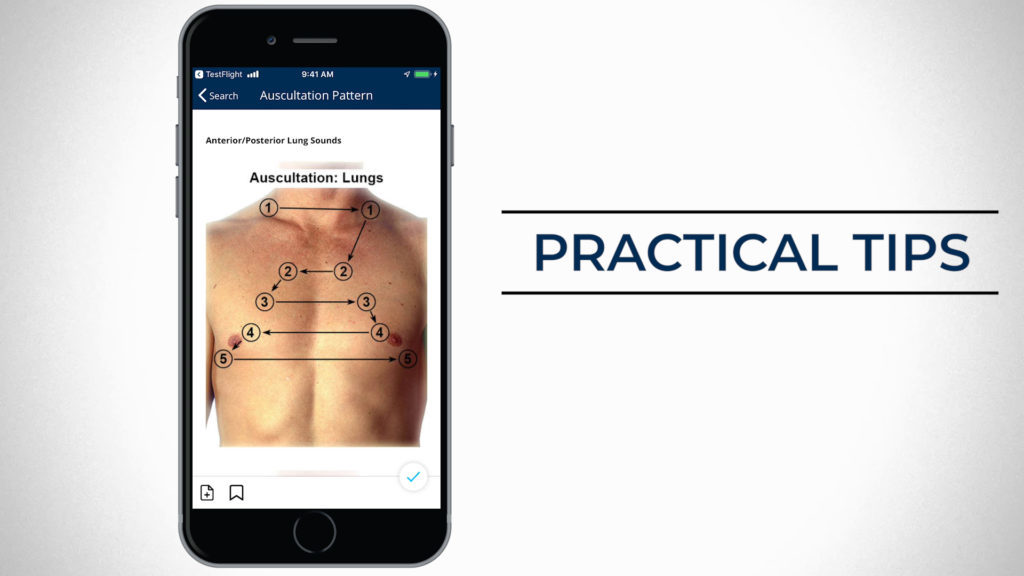
Nursing Clinical Mastery is an all-in-one App to navigate every day practice challenges.
Mobile applications to improve communication between health team members and to support clinical workflows are already in widespread use in most healthcare settings. Yet, many hospitals still frown upon portable device use at work–despite the potential to increase productivity.
Concerns about bring your own device (BYOD) use at work are valid and numerous, but so are reasons to advocate for more mobile nursing references. Some hospitals are daring to explore why their nurses love having mobile apps within their reach.
First, here are the real concerns about smartphones on the floor every nurse should know…
| Smart Phones: Potential Downsides |
| • Viewed by patients as unprofessional and unengaging • Privacy of protected health information • Distraction affecting performance and leading to errors • Lack of confidence, low staff digital literacy • Possible interference with clinical devices • Nosocomial infection transmission • Device security |
Perhaps the biggest concern is the risk for the transmission of nosocomial infection. Healthcare-acquired infections (HAI) account for large morbidity and mortality. Harmful gram negative organisms, including P. aeruginosa and Enterococcus, are often culprits for vulnerable hospitalized patients and can be carried for long periods of time on devices, including phones and ECG leads.
This is according to studies of intensive care units. (For more on HAI, just Search for whatever organism you want to learn about in the New Clinical Nursing Mastery app.) Infection control practices, including considerations for mobile devices requires focused attention and mandatory staff training, for sure.
In truth, there are a TON of personal and professional items that pose risk for contamination in the clinical environment. (How many facilities ban the use of super-cute stethoscope covers, and I wonder what’s growing on that IV med book in the med room?). And policies regarding mobile device use should address how to properly disinfect any non-critical item that could serve as a potential fomite.
But smart phones play a unique role nowadays. Why? Because mobile IT has become ubiquitous, both in personal and professional life, and for patients and nurses. Patients will gravitate more and more toward Mobile for tracking, reporting and improving health. Even more important for nurses, mobile apps have the potential to provide access to accurate data that can be applied in real-time (actionable).
Mobile IT Can Improve National Health
As of 2014, roughly 80% of Americans had access to the Internet, and more importantly, data collected from the National Institutes of Health targeting national health indicators show that over half of all adult patients access the internet most often with mobile devices. You mean our patients don’t want to wait ‘til they get home to boot up their computer and read about their new diagnosis? Just a decade ago only 6% of people reported mobile use for the same purpose, which suggests rapid adoption and widespread use.
Nurses are no different. Studies show despite the trend that nurse managers disapprove of unregulated smart phone use, the majority of next-generation nurses overwhelmingly desire to use personal handheld technology for real-time reference.
Home care nursing is in high demand because it helps control healthcare cost, and factors like these are driving research around mobile device use standards. Approximately 90% of Americans have access to a smartphone capable of accessing the Internet, and Healthy People 2020 national goals actually aim to increase mobile usage specifically for health care– so that number will surely grow. Who knew the experts actually want more patients using mobile? Why would our national plan for improving our health call for more mobile IT for patients?
The answer is simple: integrating mobile IT tools with care planning improves patient engagement and access to services and health information. It’s a pathway better self-management which is the key to improving individual and population health overall.
But apps are not just good for patients. Organizations are scrambling to find ways to get clinical references in a neat little package and in the hands of clinicians. Nurses need health information technology (HIT) to improve quality and care delivery, too. Mobile apps can offer real-time bedside or in-unit clinical decision support (CDS) for nurses, just as we do for physicians.
Clinical Decision Support (CDS) for Nurses
• Point of care prompts
• Alerts
• Electronic access to references
• Patient teaching
• Safety guidelines
Nursing Knowledge : A Vast Chasm
How many times have we been told NOT to memorize formulas and facts we need to know to care for patients? We know that the risk for errors increases in complex care environments when we don’t use resources. Trouble is…what’s out there for us?

If cell phone use has become the norm, then why DO nurses still rely on Google or physician resources? I mean, Epocrates is great–lots of cool stuff in there–so why, after 25 years working in direct patient care, do I always feel a little lost looking for a recommended drip rate or list of palliative nursing care priorities? Answer: It’s not in there. At least not in a way that’s useful to me as a nurse. I searched Up-To-Date for something the other day and gave up after an hour!
Homecare nurses tell me that accessing all the guidelines and teaching they require to do their job in the field is a challenge. What’s more, smart phones hold the potential to solve connectivity problems in rural areas, so this dilemma isn’t going away. Wouldn’t it be nice to have one application in our pockets to guide daily nursing practice?
In the age of booming telemedicine, diverse care settings, and the need for more affordable community nursing care, technology companies are waking up. Mobile references can be used to improve efficiency and reduce errors for professionals managing complex clinical conditions and home environments. So, what do nurses need? WE decided to ask some…
Any tool for nursing POC and CDS needs to integrate data from many separate sources. Nurses rely on authoritative evidenced-based organizations to guide practice such as the Centers for Disease Control and Prevention, FDA, CLIA, and OSHA along with countless nursing associations including the American Nurses Association, American Society for Perianesthesia Nurses, and American Association of Critical Care Nurses to name a few.
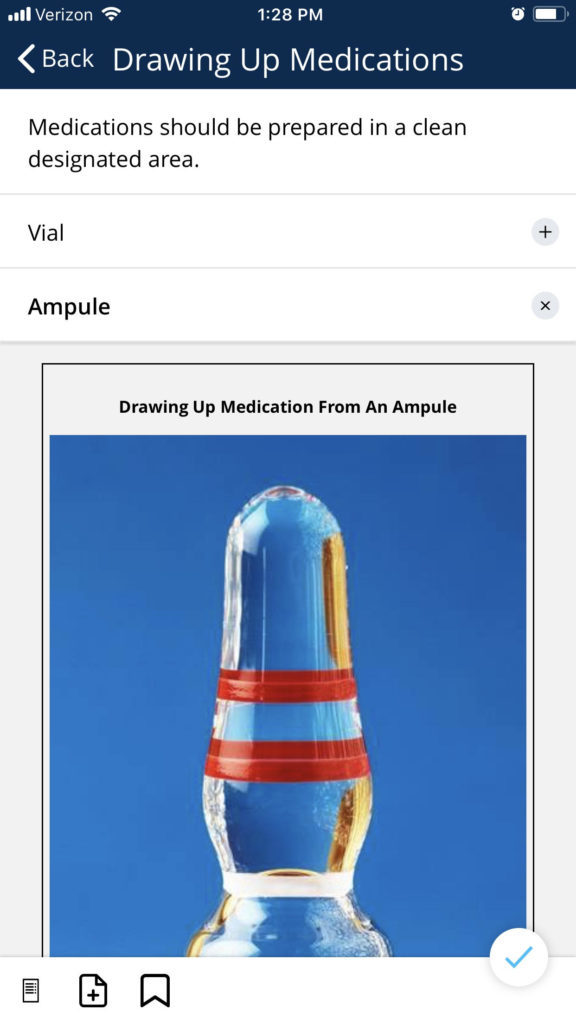
And if that is not enough, nurses require updated pharmacology references with clear guidance for medication administration and teaching. Physician references don’t always cover what nurses need to know, nor are they easily navigated–even when it comes to medications!
Nurses have become health care managers for patients and require easy access to a wide variety of guidelines and best practices that are continually updated.
Juggling complex work patterns and care settings while improving efficiency will be our biggest challenge over the next decade.
Building a comprehensive reference to compile nursing knowledge and skills for immediate access is finally within reach.
A Quest for a Nursing App to Improve Care Delivery
Some studies show nurses also have less time on the job to connect with colleagues, and spend more time alone during a shift. Yet, learning from fellow nurses is integral to our success as nurses. How do we share successes and tips for better care in such a challenging care environment?
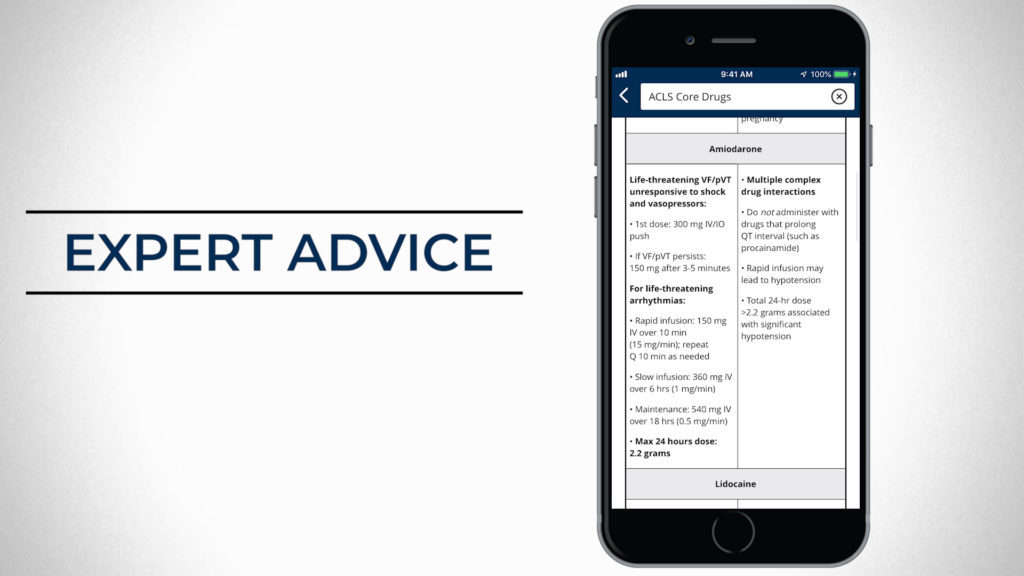
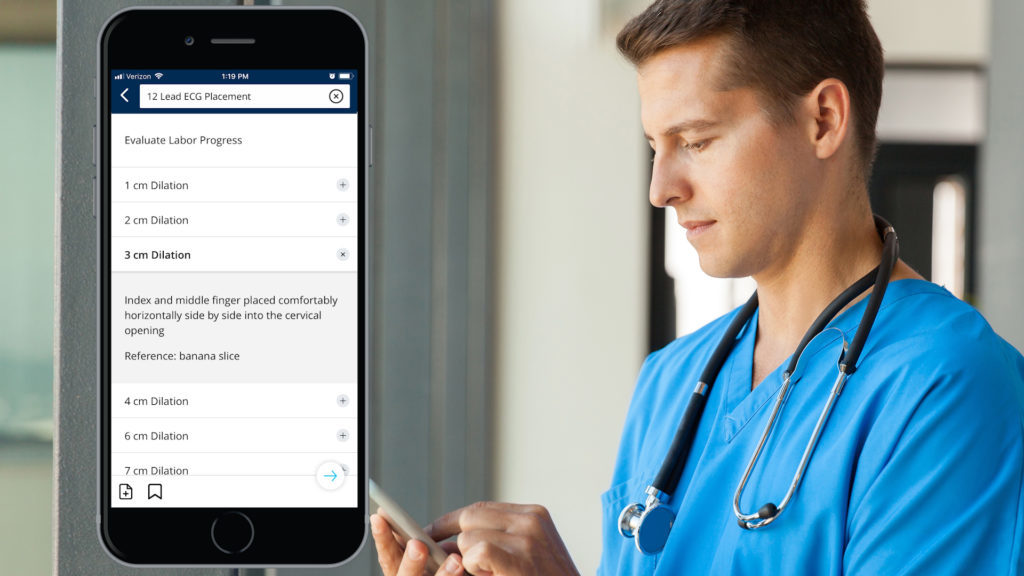
Apps for nurses are most helpful when they contain advice from expert nurses. Nursing preceptorship and mentoring is the foundation for every career transition–and nurses, new and experienced, will make many transitions throughout their lifetime. Nursing Clinical Mastery is one app that combines nursing expert advice and best practice guidelines for a unique one-stop nursing knowledge shopping experience.
Nurses may increase time spent with patients and patient satisfaction by having comprehensive references like Nursing Clinical Mastery at their fingertips on-shift and off. Float pool staff and home and community settings can benefit from tools specifically designed for nursing practice.
Promising new research has even looked at the use of mobile apps to assist with nursing skills such as wound assessment and dressing selection. The use of algorithms applied to these versatile technologies may revolutionize care delivery and improve time management and knowledge sharing.

Higher Learning Technologies, maker of award-winning nursing apps has filled the mobile reference app gap with a new offering made by nurses, for nurses. The solution, Nursing Clinical Mastery, ties evidence-based guidelines with knowledge and skills that nurses want on demand and on-the-go.
Does your facility allow personal mobile devices to help you improve your practice? Let us know! Here are some great evidence-based suggestions to promote safe mobile device use in clinical environments:
• Update cell phone use policies
• Update infection control policies to reduce fomite contamination
• Provide clear guidelines and train all staff
• Provide disinfectant wipes and encourage use
• Encourage professional cell phone etiquette
Article References
Parker, Cheryl D. "Evolution or revolution? Smartphone use in nursing practice: smartphones can aid nurses' clinical practice, but they must be used in compliance with laws, policies, and procedures." American Nurse Today, vol. 9, no. 11, 2014, p. 30+.
"Germs spread via cell phones and EKGs." United Press International, 16 Sept. 2003, p. 1008259w5583.
Loyola, S., Gutierrez, L., Avendaño, E., Severino, N., & Tamariz, J. (2018). Multidrug-resistant bacteria isolated from cell phones in five intensive care units: Exploratory dispersion analysis. Germs, 8(2), 85.
Flammia, D. (2018). Cell Phones and Bacteria…Bartholomew K. Not So Smart: Cell Phone Use Hurts Our Patients and Profession: The clinical setting is no place for divided attention. American Journal of Nursing (AM J NURS), 2018;118 (6): 11. AJN American Journal of Nursing, 118(11), 10.
Giles-Smith, L., Spencer, A., Shaw, C., Porter, C., & Lobchuk, M. (2017). A Study of the Impact of an Educational Intervention on Nurse Attitudes and Behaviours Toward Mobile Device and Application Use in Hospital Settings. Journal of the Canadian Health Libraries Association (JCHLA), 38(1), 12–29.
Snoots, L. R. (2016). Use of Personal Electronic Devices by Nurse Anesthetists and the Effects on Patient Safety. AANA Journal, 84(2), 114–119.
Mather CA, Gale F, Cummings EA. Governing mobile technology use for continuing professional development in the Australian nursing profession. BMC Nursing. 2017;16:1-11.
Depatie, A., & Bigbee, J. L. (2015). Rural Older Adult Readiness to Adopt Mobile Health Technology: A Descriptive Study. Online Journal of Rural Nursing & Health Care, 15(1), 150–184.
Jun, Y. J., Shin, D., Choi, W. J., Hwang, J. H., Kim, H., Kim, T. G., … Hong, J. P. (Jp). (2016). A Mobile Application for Wound Assessment and Treatment. International Journal of Lower Extremity Wounds, 15(4), 344–353.
