On the forefront of nursing care, we are now challenged to relieve pain and suffering while preventing narcotic addiction. This is an overwhelming goal for all healthcare staff. Let's take a look at the problem.
In the 1990s, the pain scale became the sixth vital sign in nursing. We were reassured that offering pain relief using narcotics would not result in addiction for our patients.
Patients began to believe that complete pain relief was not only an option, but an expectation.
The new script must include realistic pain relief goals.
Who doesn't want to be pain free? Zero pain on a 0-10 numeric pain scale is not achievable, nor desirable, for the majority of patients. Pain serves to keep the fresh post-op patient from overexertion and injury, for example.
We now know that up to 30% of patients will misuse prescribed narcotics. When the patient can no longer obtain refills for prescribed medications, 10% of people may turn to other sources of relief.
80% of heroin users experience opioid misuse first (NIH, 2018).
Habit is habit, and not to be flung out of the window by any man, but coaxed downstairs a step at a time.
Mark Twain
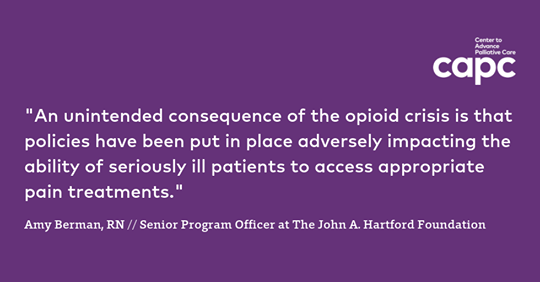
Prescribers require ongoing education in evolving practices for pain relief. Insurance often limits or denies coverage for alternative relief methods, even evidence-based therapies like massage (ANA, 2018).
Patients need to be relieved of the shame of seeking pain relief. Patients under-report pain to avoid feeling judged or over-report pain to obtain adequate relief.
What is addiction, really? It is a sign, a signal, a symptom of distress. It is a language that tells us about a plight that must be understood.
Alice Miller
Pseudoaddiction begins with the inability to get pain relief. The patient escalates their behavior to convince others that the pain is real. Then the patient develops a mistrust of the healthcare team, leading to agitation and addiction behaviors.
Tolerance
Dependence and tolerance represent a normal biological response to a substance. They are the physical results of a drug’s use when taken as prescribed to support a reasonable quality of life for acute or chronic conditions.
Examples of dependence and tolerance exist in our everyday life - daily coffee, diet Coke, Cold Brew, Monster. Without that caffeine, the person experiences withdrawal symptoms such as headache and agitation. With prolonged use, the person needs an extra cup to get the desired effect.
Tolerance is a diminished response to a drug after repeated use. For example, a patient who uses Oxycontin (oxycodone ER) for chronic pain relief may begin needing 10 mg doses.
Tolerance means the patient will become used to this Oxycontin dose, and it will no longer be effective, requiring 20 mg, then 60 mg, and so on.
A narcotic dose ceiling is only limited by its adverse effects, such as respiratory depression, and when it is titrated correctly, adverse effects do not occur or mild side effects occur and resolve quickly.
Dependence is a physical state of the body’s adaptation to the presence of a drug. This can occur quickly. For example, the patient who receives Dilaudid (hydromorphone) every two hours over a one week period for ongoing acute pain will experience dependence.
Dependence means that when the patient is discharged, they will experience mild withdrawal symptoms as the body adjusts to the absence of the opioid.
While tolerance and dependence are a component of addiction, their presence does not equal addiction.
Addiction
Addictions ... started out like magical pets, pocket monsters. They did extraordinary tricks, showed you things you hadn't seen, were fun. But came... to make decisions for you. Eventually, they were making your most crucial life-decisions. And they were ... less intelligent than goldfish.
William Gibson
At first, addiction is maintained by pleasure, but the intensity of this pleasure gradually diminishes and the addiction is then maintained by the avoidance of pain.
Frank Tallis
Psychological dependence, addiction, interrupts normal life. It is a struggle that nurses and prescribers face: determining who is drug seeking and who needs pain relief.
In emergency departments, pain accounts for about 40% of visits. Up to 20% of emergency department visits may be due to drug-seeking, though.
The healthcare team is tasked with determining who needs pain relief and who needs addiction relief.
Possible drug seeking behaviors:
- The patient passed hospitals near them to get to yours.
- The patient has seen multiple doctors in a short time.
- The patient has multiple pharmacies.
- The patient will only accept a narcotic dose.
- The patient appears to exaggerate symptoms for others.
- The patient reports conditions that are difficult to objectively evaluate.
- The patient insists that their pain is a 10, 11, or 12.
- The patient insists the pain med be administered IV.
Regardless, even "classic" drug-seeking behaviors are not reliable indicators. Pseudoaddiction can also cause these behaviors as the patient tries desperately to get relief from pain. This can leave healthcare staff in quite a dilemma.
Addiction identification and good pain relief is an area of continued development and trial-and-error.
For those with a history of addiction and who are actively experiencing pain, the problem is incredibly complex.
Ineffective pain management by reluctant prescribers can cause pseudoaddiction, doctor shopping for multiple prescriptions, illegal drug use, and leave patients suffering (ANA, 2018).
We are obliged to find the compromises so that patients can get relief, whether from pain, tolerance and dependence, or addiction.

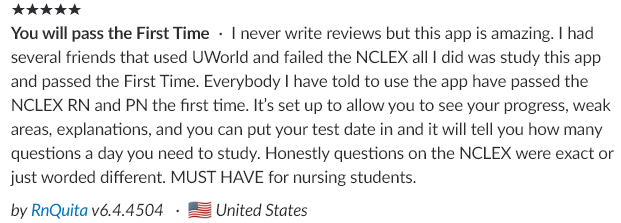
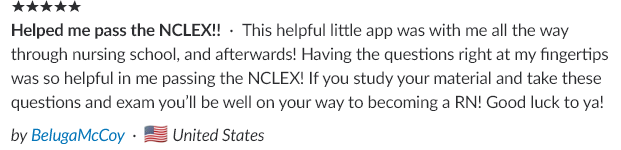
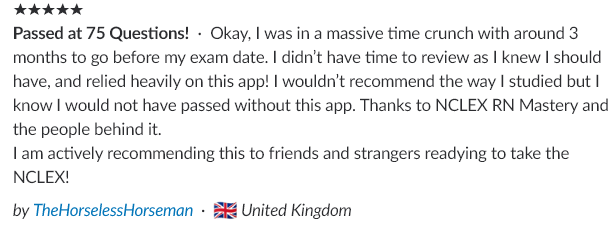
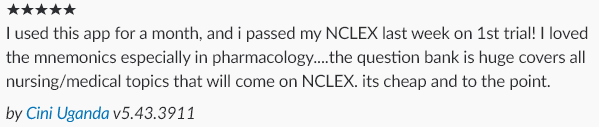
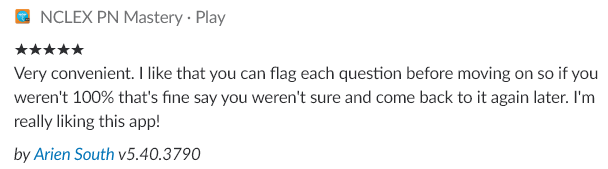
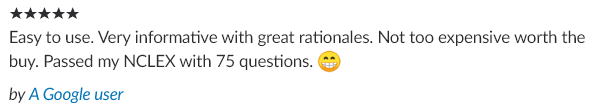
Connect with our nursing community
See what users are saying about our Nursing Mastery products!
Other resources for understanding addiction
ANA (2018). The opioid epidemic: The evolving role of nursing. American Nurses Association, Issue brief, 1-14. Retrieved from https://www.nursingworld.org/~4a4da5/globalassets/practiceandpolicy/work-environment/health--safety/opioid-epidemic/2018-ana-opioid-issue-brief-vfinal-pdf-2018-08-29.pdf
Bettinardi-Angres, K. & Angres, D. (2010). Understanding the disease of addiction. Journal of Nursing Regulation 1(2), 31-37. Retrieved from https://www.ncsbn.org/Understanding_the_Disease_of_Addiction.pdf
Goldman, B. (2012). Neuroscience of need: Understanding the addicted mind. Stanford Medicine. Retrieved from http://sm.stanford.edu/archive/stanmed/2012spring/article5.html
Grover, C. (2012). Quantifying drug-seeking behaviors in the emergency department. Physician’s Weekly. Retrieved from https://www.physiciansweekly.com/drug-seeking-behaviors-emergency-department/
Grover, C., Elder, J., Close., R., Curry, S. (2012). How frequently are “classic” drug-seeking behaviors used by drug-seeking patients in the emergency department. Western Journal of Medicine, 13(5), 416-421. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3556950/
HHS (2018). The opioid epidemic by the numbers: 2016 and 2017 data. U.S. Department of Health and Human Services. Retrieved from https://www.hhs.gov/opioids/sites/default/files/2018-09/opioids-infographic.pdf
Inspire Malibu (2018). Understanding addiction reward and pleasure in the brain. Inspire Malibu. Retrieved from https://www.inspiremalibu.com/blog/alcohol-addiction/understanding-addiction-reward-and-pleasure-in-the-brain/
Luthi, S. (2018). House passes opioids legislation. Modern Healthcare. Retrieved from https://www.modernhealthcare.com/article/20180928/NEWS/180929882
NCADD (2015). Understanding addiction. National Council on Alcoholism and Drug Dependence. Retrieved from https://www.ncadd.org/about-addiction/drugs/understanding-addiction
NIH (2018). Understanding drug use and addiction. National Institute on Drug Abuse. Retrieved from https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction
NIH (2018). The science of drug use and addiction: The basics. National Institute on Drug Abuse. Retrieved from https://www.drugabuse.gov/publications/media-guide/science-drug-use-addiction-basics
NIH (2018). Opioid overdose crisis. National Institute on Drug Abuse. Retrieved from https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
Ray, S. & Hoffman, K. (2018). Opioid stigma is keeping many cancer patients from getting the pain control they need. STAT. Retrieved from https://www.statnews.com/2018/07/06/cancer-patients-pain-opioid-stigma/