Non-communicable diseases (NCDs)
Non-communicable conditions such as cardiovascular disease, diabetes, cancers, and chronic respiratory illness cause over half of the deaths every year worldwide, according to the WHO. It's almost a certainty that most of your clients will have not one, but multiple, non-communicable diseases (NCDs).

To oversimplify, cancer can often be attributed to increased chemical use and exposure in our everyday life and the sheer fact that we live longer now than in the last century. The same factors contribute to respiratory issues. These are serious and complex issues, or the WHO wouldn't prioritize them. However, when we look at individual and controllable risk factors, factors the nurse can affect in every-day interactions, we really have to focus on cardiovascular disease and diabetes.
Many clients with diabetes (specifically DM II) also have cardiovascular disease (CVD), and if they do not yet, they may have both soon! How do these two classes of NCDs affect each other? What does the nurse do about this epidemic?
See that crazy yummy Luther Burger? — Beef, bacon, cheese, glazed doughnut, and a side of deep-fried potatoey goodness with nary a real vegetable in the picture. Is this THE problem causing cardiovascular and endocrine disorders? No, of course not. NCDs are occurring at increased rates worldwide including areas where these foods may not be readily available.

However, seventy years ago, pinto beans and collard greens was a standard meal, working the farm was a daily activity, and getting an orange or nuts was a special and expensive treat reserved for holidays. Nevermind how rare a treat Pop Tarts or a Moon Pie was until the last quarter of the last century. This is a fact - times actually have changed. Just as we are starting to live longer with vaccines and anti-infective medications, the mortality rate is increasing due to a different lifestyle!
What does the nurse understand?
There are lots of theories about this phenomenon - modern day stress (and the HPA axis and PNE — topics for another day or degree!), overeating, an abundance of nutrition-poor but cheap foods, reduced physical work. Really, it is a combination of these factors and more. There is also the question of what comes first? Surely obstructive sleep apnea can cause all of these other listed conditions; so could obesity, though. Diabetes induces each of the other conditions, too. Where do we start?
The interactions and feedback loops are known. This might be referred to as metabolic syndrome, a cluster of conditions including high blood pressure and sugar, excess fat, and abnormal lipid metabolism. This cluster is often also accompanied by, or leads to, gastroesophageal reflux, nicotine addiction, or other complicating factors.
[caption id="attachment_2618" align="alignnone" width="732"]
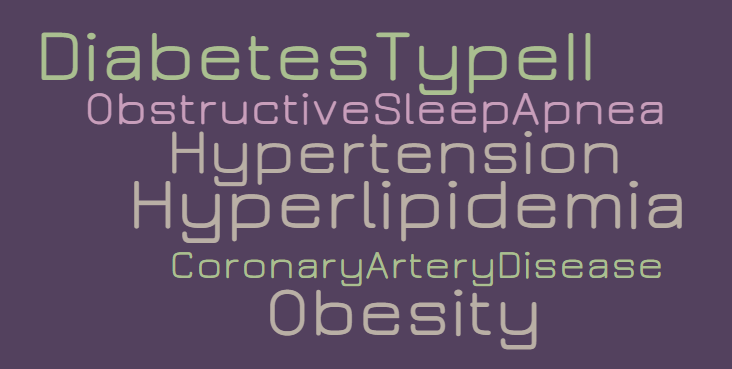
This is a common condition combination for this half of the 21st century.[/caption]
Diabetes can lead to cardiovascular disease, macrovascular problems (the kind that leads to a heart attack or stroke), microvascular problems (like blindness), and vascular damage in the kidneys, too, leading to kidney disease. If that is not enough, diabetes leads to nerve damage in the extremities, which causes annoying or painful tingling in the hands and feet, and in the gastrointestinal system, leading to reflux, constipation, and bloating.

When explaining the pathophysiology related to the effects of diabetes on cardiovascular disease, I find this imagery useful: Imagine forcing small cubes of sugar through a large drinking straw repeatedly. First the straw is just scratched up a bit and sometimes the sugar needs to be diluted to pass through effectively, but eventually the straw is shredded, right? That happens in the vascular system, too, except the body sends clots to repair the scratches and damage. This is just the start of how diabetes (the sugar cubes) and the cardiovascular system (the drinking straw) interact.
CVD and DM are a deadly combination. There is evidence that CVD and heart attack incidence could be reduced by 60% - 80% if lifestyle modifications occur. Repeatedly, we hear that taking the first step is the most difficult. How can we help people get started and keep going?
What does the nurse do?
Meet them where they are.
People are in different states of readiness for change and in understanding. It is important to find out what they understand and what they think they are able to do. From this standpoint, the nurse can work with the patient to build a plan.
Address barriers.
Decreased self-motivation, depression, busy/work/kids, love of sodas or burgers, too busy to cook, eating in a rush, eating large portions, home support, procrastination, jobs that require sitting, disabilities, exhaustion....
Plans have to be individualized and targeted. It is never enough to tell someone to "eat less sugar," "just work out 3 times each week," or "eat more vegetables." (If you didn't know it already, lots of folks consider potatoes a vegetable and have no clue that a plate of spaghetti turns into sugar.)
People need guidance, mentoring, and accountability regarding what those things mean in their lives. Few people come to the health care provider without already knowing, for example, that they are obese and need to eat better and work out more. If they could figure out how to make that work for them, they would have, perhaps. It is the role of the professional to assist in making those goals tangible.
Set goals.
Daily glycemic targets and a controlled HbA1c are important. Make suggestions for alternative foods or recipes.
For the person who just loves a piece of chocolate cake each night, your goals to reduce carbs will not matter. Ask if it is reasonable to have cake every other night to start. Create targets and strategies together.
Maybe they feel more tired when their glucose levels are less than 110 mg/dL, and they feel better when their glucose is 140-160 mg/dL. Work with that information to create goals!
Nutrition plays a huge role in reducing cardiovascular disease! Working with the patient to understand what glycemic targets mean for their daily choices is more important than the targets themselves.
For the person who thinks corn and carrots are the best vegetables and grapes are their favorite fruit, more guidance will be needed. Very few people can be motivated enough to make a direct swap between corn and brussel sprouts.
What portions and frequency of favorite foods is mutually acceptable? Where can new foods best be incorporated? Make simple changes and easy wins - busy in the morning and grabbing a doughnut? Swap it out with peanut butter-heavy wheat toast. Is peanut butter ideal? Of course, not. Is it better than a doughnut? Yup, sure is.
Activity sounds like an easy addition. As a nurse, YOU know that isn't so! Nurses who have great workout routines are weight lifting at 3:30 in the morning before a 12-13 hour shift. UGH!
If 30 minutes, 3 times per week (the standard recommendation) is out of the question, how about 15 minutes, 6 days per week? Building the habit may be the most difficult hurdle. Starting somewhere is better than not starting at all. Your patient will still be doing laps around the folks still stuck to the couch!
Lots of people think they need a gym membership. Clarify any misconceptions! Suggest grabbing a stationary bike at yard sale for $20 to get moving! Suggest taking the stairs for one floor at work rather than for 7 floors. It doesn't have to be all or none—that would make anyone feel defeated!
Reduce comorbidities
Smoking. Hypertension. Hyperlipidemia. Weight. Stress.
The patient needs a plan for quitting tobacco, knowing they may need to try multiple plans and multiple times to be successful is important, too. Anyone with diabetes should be on (or have been considered for) a mild dose of antihypertensive like lisinopril for kidney protection and maybe an anti-lipid medication or fish oil, and the nurse is in a prime position to ensure those prescriptions are available and understood.
For the patient with mild stress, adding physical activity may be enough to manage it. For the patient with severe stress, a combination of medication and therapy may be needed. The nurse makes sure to at least address these issues as often as is needed to help the patient succeed.
Teach and support.
Changing the risk factors associated with noncommunicable diseases is not simple. Unless the nurse encounters the client at the time of a brand new diagnosis, chances are good that whatever is cliche about diet, exercise, and healthy habits is something they have heard many times. Offer a variety of support systems such as weight loss centers, apps, books, and groups. Teach and reteach. Health is a journey, not a destination. Be a dedicated tour guide.
References and Images
https://www.americannursetoday...
https://journals.lww.com/tnpj/...
Smog: By Tasnim News Agency, CC BY 4.0, https://commons.wikimedia.org/...
Sugar: david pacey By david pacey from LEEDS, West yorkshire - Sugar Cubes, CC BY 2.0, https://commons.wikimedia.org/...
Luther Burger:




